Optic Neuromyelitis Or Devic’s Disease: What Is It?
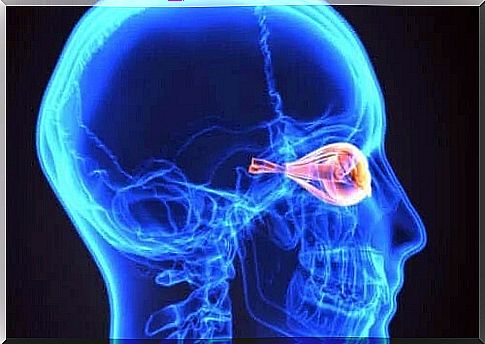
Autoimmune diseases are a group of pathologies in which the cells responsible for defending the body attack their own organs. This is also the case in optic neuromyelitis (NMO), a disease that involves demyelination of certain areas of the central nervous system (CNS).
A substance called myelin covers the entire CNS and is involved in the proper transmission of nerve impulses. In the case of optic neuromyelitis, specific antibodies will attack the proteins in the spinal cord and optic nerve, aquaporins 4, altering their proper functioning.
This condition is also known as Devic’s disease and has a recurring form of presentation. In fact, recurrences occur in 70% of cases. The most common symptoms are changes related to inflammation of the optic nerve and spinal cord.
Similarities and differences between optic neuromyelitis and multiple sclerosis
Multiple sclerosis (MS) is an autoimmune disease that also attacks the central nervous system, facilitating confusion with NMOs. In fact, for many years, experts considered optic neuromyelitis to be a type of multiple sclerosis.
The two pathologies in question affect the structures that make up the central nervous system, causing demyelination. Both affect the spinal cord. However, while MS is able to alter different brain structures, NMO only affects the optic nerve.
The symptoms presented by patients are very similar, because both diseases have recurrent forms. People with multiple sclerosis also experience optic neuritis and myelitis, so visual and sensory problems are common.
The main difference between the two diseases is the humoral alteration present in the case of optic neuromyelitis. Studies have shown that most patients with NMO have anti-aquaporin antibodies 4, which are very rare in people with MS.

Symptoms of optic neuromyelitis
Diagnosis of optic neuromyelitis
One of the main findings guiding the diagnosis of optic neuromyelitis is the presence of anti-aquaporin 4 antibodies in the bloodstream. These antibodies are found in more than 70% of patients. Therefore, they are a clear indication.
These molecules are responsible for the destruction of aquaporin 4 in the CNS and subsequent demyelination. Although it is a recent discovery, it has proven useful in early diagnosis.

Treatment of optic neuromyelitis
The symptoms of the disease appear as a result of an inflammatory process. Therefore, the use of corticosteroids helps to reduce the impact of the disease. This type of medication also prevents recurrence.
When corticosteroids fail to improve symptoms, a plasma exchange may be necessary. This procedure involves removing blood from the body and then separating the plasma or fluid from the cells and replacing it with a synthetic analogue.
Plasma exchange is a process that can take hours and must be performed several times. Finally, the doctor prescribes immunosuppressive drugs. They decrease the activity of the immune system, thus reducing damage to the CNS structures.
NMO: A difficult disease to diagnose
In conclusion, optic neuromyelitis is a degenerative autoimmune disease with ocular and neurological symptoms. Although this pathology is easily confused with other CNS diseases, diagnostic methods have advanced greatly.
Unfortunately, there is no specific treatment for this disease. However, corticosteroids and immunosuppressants help the patient feel better. People with NMOs need to make lifestyle changes to prevent progression and relapse.